By: Yijian Yang
The reality: In Canada, an increasing frail population of older adults reside in long-term care facilities (Postl et al., 2011), and more than 50% of them will fall each year (Rubenstein et al., 1994). Falls are the leading cause of injury-related death in older adults (Stevens et al., 2006).
Ideally, when an older adult in long-term care presents with a fall, the care management team would design a personalized fall management plan specific to the circumstances of the fall, including consideration of tailored exercise program, assistive device prescription, or environmental modification that address the perceived cause of the fall (Rubenstein, 2006). Because a personalized approach may be resource intensive, an alternative and perhaps more feasible strategy would be to customize the program based on factors such as sex, age, and clinical status.
What information do we need for fall prevention? To prevent falls, we need to understand “how” older adults fall. However, a major challenge is the lack of objective information about fall incidence. Previous research has mostly been based on self-reports or interviews from witnesses, which may lack accuracy (Cummings & Nevitt, 1988; Yang et al., 2015). Different than other research, we used an innovative research approach to study falls based on observations of real-life falls (Robinovitch et al., 2013). This eliminates the bias caused by self-reports.
Specially, we used digital video cameras to capture falls that occurred in common areas (such as dining rooms, hallways, and lounges) inside two long-term care communities (Figure 1). Each video was analysed by a team of three experts to determine the causes of imbalance and the activities at the time of falling. We also collected data on the health status of the participants. Statistical models were used to examine how fall circumstances associated with age, sex, and health status.
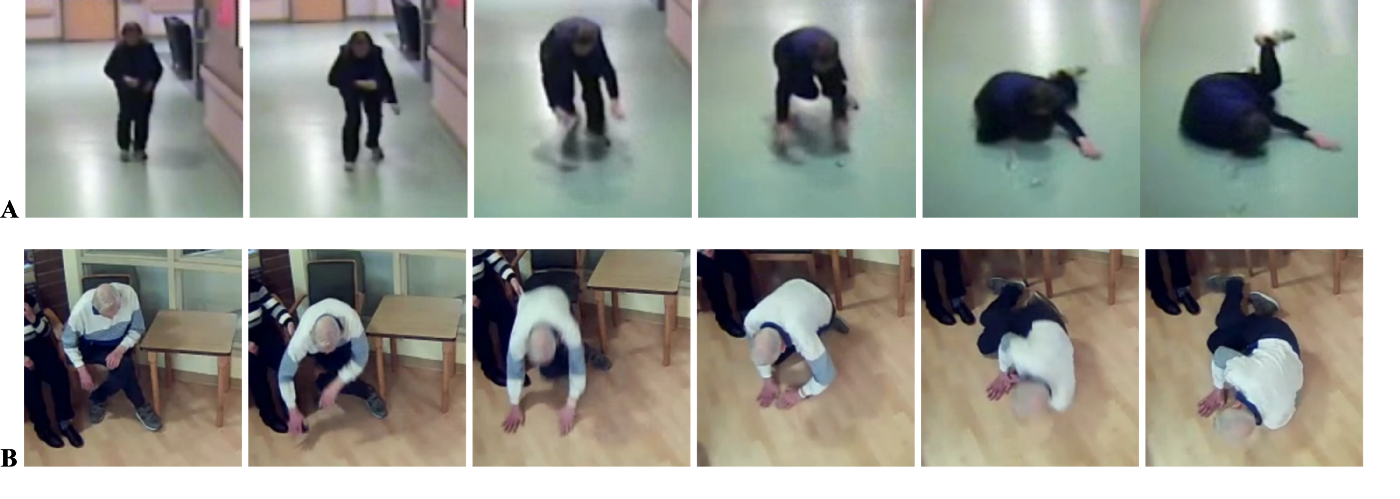
Figure 1. Snapshots from video footage of falls experienced by: (A) a 77-year old woman who tripped during walking. She fell forward but rotated during descent to land the right side of her pelvis and torso; (B) an 86-year old man who lost balance by sliding off a chair while seated. He fell forward, used his hands to arrest the fall, and rotated his body during descent to land sideways.
Research revealed the differences in falls between men and women:
· What activity were men and women doing at the time of falling? The researchers found that men were nearly 1.5-times more likely than women to fall while seated or getting up. However, women were 1.6-times more likely to fall while walking (Figure 2).
· How did men and women lose balance? Men were 1.4-times more likely than women to fall from loss of support with an external object, such as a cane or a walker. On the other hand, women were 1.4-times more likely to fall due to trips or stumble (Figure 2).
· What was the influence of health status on falls? Regardless of sex, falls from loss of support were more common among individuals who were less independent in activities of daily living, who used more medications, and who used a diuretic. Individuals with independent activities of daily living and intact cognition were more likely to fall while walking, but less likely to fall while seated or while rising.
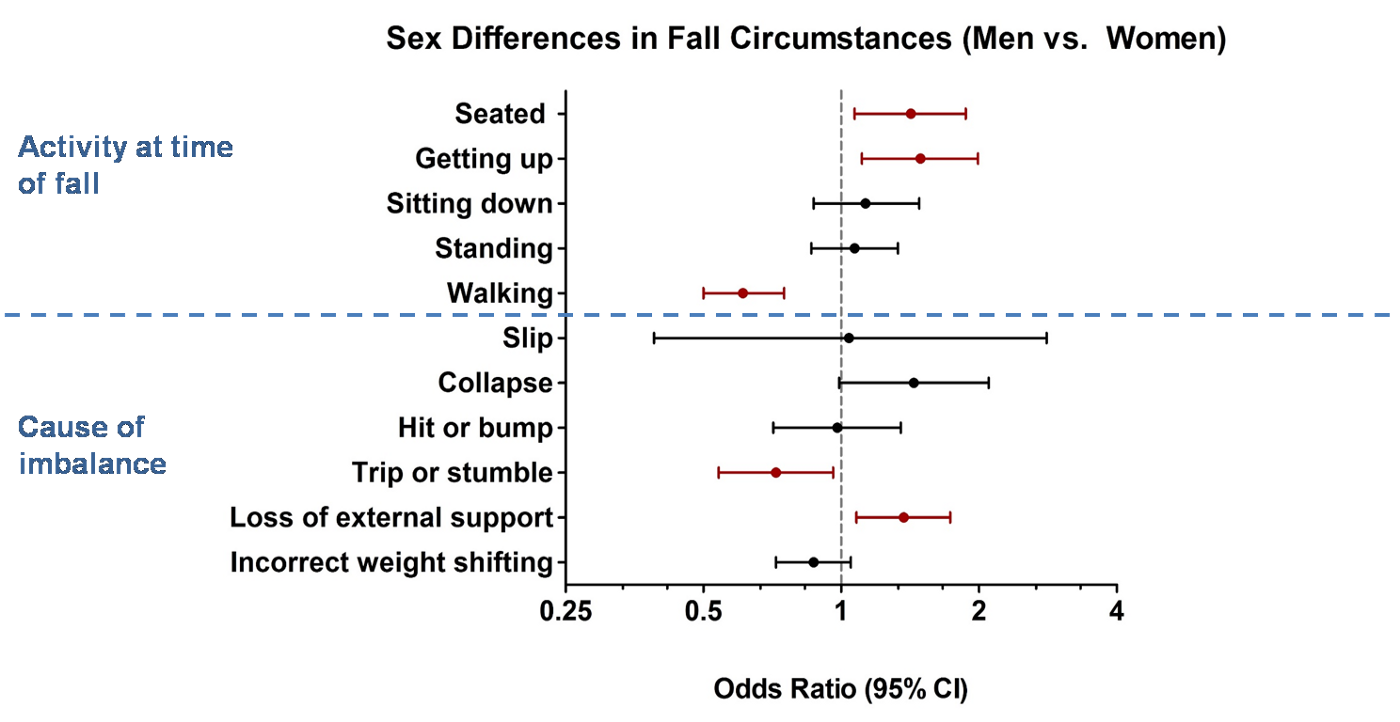
Figure 2. Comparison of fall characteristics of men vs. women (n = 529, with 1738 falls). An Odds Ratio (middle dot of each line) larger than 1 represents a higher risk of falling due to the activity or cause of imbalance among men compared to women. An Odds Raito lower than 1 represents a lower risk. Red color refers to statistically significant.
Implication — from research to real life
Although rates of falls are similar in men and women (Campbell et al., 1990), our research found that men and women fall differently in the long-term care setting. This may be due to the physiological and behavioural differences between older men and women (James & Parker, 1989; Avlund et al., 2003). When compared with women, older men are more sedentary and have low social participation; both are associated with mobility disability (Avlund et al., 2003; Paffenbarger et al., 1993).
The sex differences in falls and the influence of health status on falls can guide the basis of change within long-term care communities. Changes might include:
- Customizing exercise programs for men and for women, as well as programs tailored to degree of physical function.
- Reminding residents to lock their wheelchairs while transferring and aiding those who are unable to transfer independently to or from a wheelchair.
- Systematically reviewing medication and enhancing supervision for residents who are physically dependent.
- Increasing supervision for residents who exhibit aggressive behavior.
Finally, communities can use their own video cameras or wearable sensors to monitor activity levels and quality of performance to reveal mobility patterns among older men and women, which can be used to help design exercise programs for falls prevention in local communities.
Reference of this paper
Yang, Y., van Schooten, K., Sims-Gould, J., McKay, H.A., Feldman, F., and Robinovitch, S.N.: Sex Differences in the Circumstances Leading to Falls: Evidence from Real-life Falls Captured on Video in Long-term Care. Journal of the American Medical Directors Association (JAMDA). Feb 2018; 19(2):130–135.
References:
Avlund K, Vass M, Hendriksen C. Onset of mobility disability among community-dwelling old men and women. The role of tiredness in daily activities. Age Ageing 2003; 32:579e584.
Campbell AJ, Borrie MJ, Spears GF, et al. Circumstances and consequences of falls experienced by a community population 70 years and over during a prospective study. Age Ageing 1990; 19:136e141.
Cummings SR, Nevitt MC, Kidd S. Forgetting falls. The limited accuracy of recall of falls in the elderly. J Am Geriatr Soc 1988; 36:613e616.
James B, Parker AW. Active and passive mobility of lower limb joints in elderly men and women. Am J Phys Med Rehabil 1989; 68:162e167.
Paffenbarger RS Jr, Hyde RT, Wing AL, et al. The association of changes in physical-activity level and other lifestyle characteristics with mortality among men. N Engl J Med 1993; 328:538e545.
Postl B, Wright J, Boileau L, et al. Health Care in Canada 2011, A Focus on Seniors and Aging 2011, Canadian Institute for Health Information: Ottawa, 2011.
Robinovitch SN, Feldman F, Yang Y, et al. Video capture of the circumstances of falls in elderly people residing in long-term care: An observational study. Lancet 2013; 381:47e54.
Rubenstein LZ, Josephson KR, Robbins AS. Falls in the nursing home. Ann Intern Med 1994; 121:442e451.
Rubenstein LZ. Falls in older people: Epidemiology, risk factors and strategies for prevention. Age Ageing 2006; 35:ii37eii41.
Stevens JA, Corso PS, Finkelstein EA, Miller TR. The costs of fatal and non-fatal falls among older adults. Inj Prev 2006; 12:290e295.
Yang Y, Feldman F, Leung PM, et al. Agreement between video footage and fall incident reports on the circumstances of falls in long-term care. J Am Med Dir Assoc 2015; 16:388e394.