But do older adults have easy access to programs that keep them active?
By Samantha Gray
Public health messages are clear — we all need to add more physical activity into our lives. As we age, this message focuses on physical activity to keep us healthy, and hopefully prevent catastrophic health events. I am a PhD student focused on the promotion of healthy aging at the population level. I know of many (many) studies of physical activity programs designed specifically to help older people prevent falls, stay mobile and independent, prevent chronic disease, and a host of other stuff that ostensibly improves health.1,2,3 What I am learning now is that most of these effective physical activity programs NEVER make it out into the real world. They are primarily one-off studies conducted by researchers in academic ivory towers. How then can they actually help older people? So, I set out to answer this question:
If an effective intervention never leaves a controlled research environment, is it truly effective?

To answer this daunting question, I delved into a field of academic study called Implementation Science. Simply speaking, Implementation Science is the study of taking effective health innovations and learning how best to help people/organizations in vastly different places deliver (e.g., implement) those innovations to more and more different groups of people.4,5 Learn more here. To illustrate — say I want to know if I can successfully implement an effective chair fitness class (let’s call it ‘Get Fit while I Sit’) to older adults who live in three different regions of Canada. The implementation scientist in me will ask questions6 at a couple of levels. First, I want to know;
· Do those delivering ‘Get Fit while I Sit’ have the resources, training, and skills they need to implement effectively? [capacity]
· Are implementation strategies acceptable, feasible, appropriate to organizations that are going to deliver ‘Get Fit while I Sit’ to their members and for the different regions where classes will be delivered?
I also would want to know;
· How much of ‘Get Fit while I Sit’ was delivered by the chair fitness instructor? [Dose delivered]
· How well did the instructor deliver it? [Quality]
· How widely was it delivered? [Reach]
Armed with implementation science principles, I plunged into the scientific literature. My mission: to find out just how many of these great physical activity programs evaluated the questions I posed above. I searched for:
- any indicators (measures) of how the program was implemented;
- the number of programs that were guided by frameworks within the implementation science field; and
- the number of programs that achieved widespread delivery (scaled-up) and were broadly accessible to older people.
With some (lots of) help from my colleagues, I took a rigorous and systematic approach.7 Our team screened more than 2400 published papers that described physical activity and exercise programs that were designed and implemented for community-dwelling older adults. We narrowed this pool down to 159 publications, representing 137 unique studies, that met our *criteria.
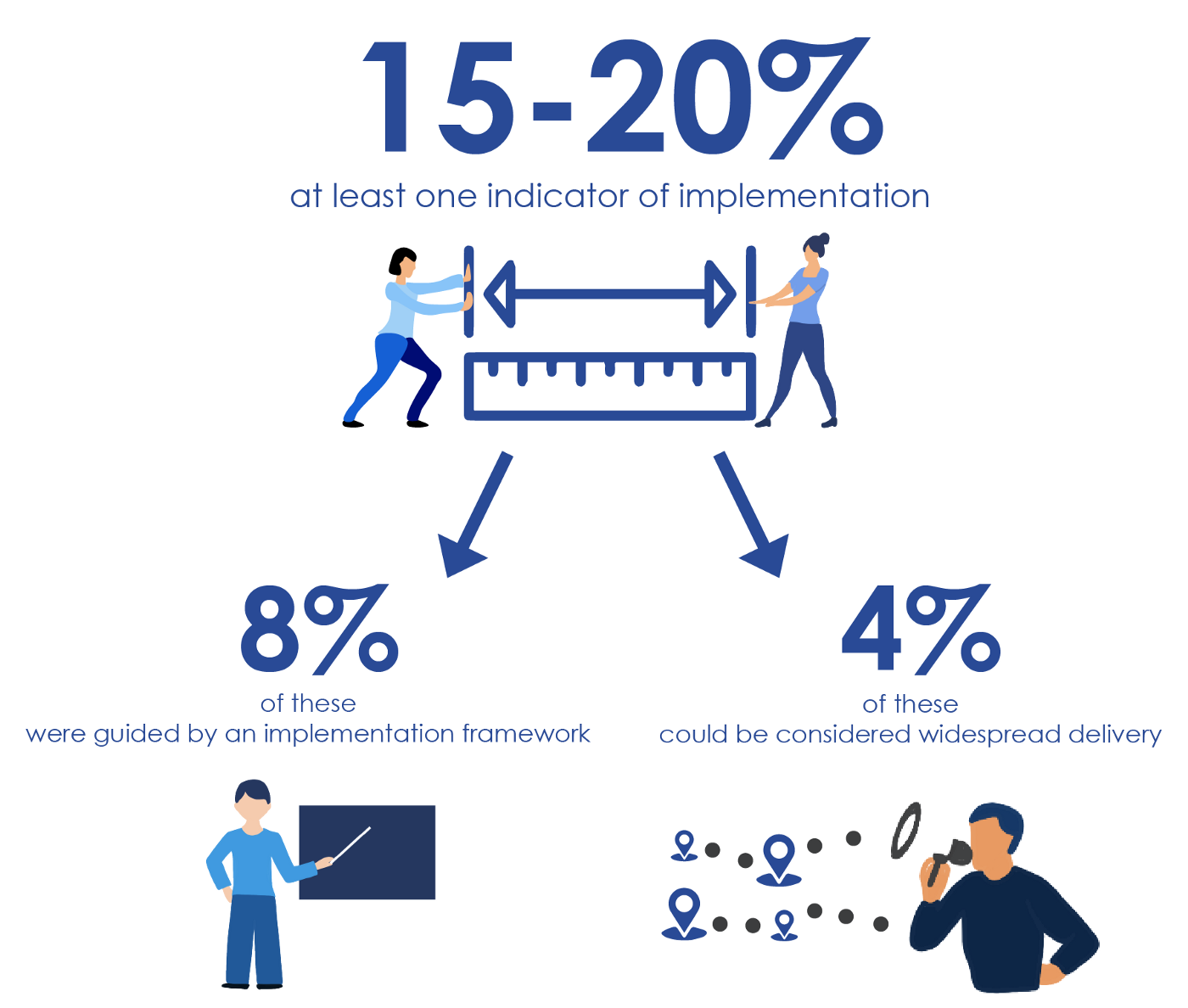
So how many of these studies actually reported at least one indicator of implementation? [Drum roll] Only 15–20%. The most common indicator assessed in these studies was ‘dose received’. Dose received measured attendance at the program or compliance with the program (reported in 114 studies; 83%). Only 8% of studies were guided by an implementation framework (defined as ‘a structure, overview, or outline of various concepts or variables and the relations between them that are presumed to account for a phenomenon’).8 This is a little dismal, considering that there are more than 60 published frameworks to guide researchers on how to deliver effective programs successfully and at scale.9 Finally, only 6 studies (4%) had what could be considered widespread delivery (were scaled-up). A disappointing finding indeed. I was dismayed that vastly more resources are invested in developing ‘one-off’ innovations (interventions/programs/practices) than are invested in discerning how to deliver them effectively and broadly so that they can benefit a larger number of people.
Did I answer my question ‘do older adults have easy access to programs that keep them active?’ In short, yes I did. There are tons of effective physical activity programs out there for older adults. But few make it out of controlled research settings and into the community where they can be delivered to and easily accessed by older adults. But, there is a way forward and I would be remiss if I did not conjure up the words of Stephen Covey ‘begin with the end in mind’. I defer also to the World Health Organization that recommends that from the start we build health initiatives that can be easily scaled-up so that they reach more people in more places. Initiatives must also be designed to be readily adaptable to diverse contexts and communities.10 As researchers we can only get this done if we work closely with key community partners who are familiar with the places (and the people) where we wish to launch our program. In a nutshell, it is time to sort out widespread delivery — how best to scale-up — effective programs so that more older adults access them to keep moving and grooving.
References
1. Zubala A, MacGillivray S, Frost H, et al. Promotion of physical activity interventions for community dwelling older adults: A systematic review of reviews. PLoS One. 2017;12(7):1–36. doi:10.1371/journal.pone.0180902
2. Paterson DH, Warburton DE. Physical activity and functional limitations in older adults: a systematic review related to Canada’s Physical Activity Guidelines. Int J Behav Nutr Phys Act. 2010;7:38. https://www.ncbi.nlm.nih.gov/pubmed/20459782.
3. Bauman A, Merom D, Bull FC, Buchner DM, Fiatarone Singh MA. Updating the evidence for physical activity. Gerontologist. 2016;56(S2):S268–80. https://www.ncbi.nlm.nih.gov/pubmed/26994266.
4. Eccles MP, Mittman BS. Welcome to Implementation Science. Implement Sci. 2006;1(1). doi:10.1186/1748–5908–1–1
5. Curran GM. Implementation science made too simple: a teaching tool. Implement Sci Commun. 2020;1(1):1–3. doi:10.1186/s43058–020–00001-z
6. Brownson RC, Colditz GA, Proctor EK. Dissemination and Implementation Research in Health: Translating Science to Practice. 2nd ed. New York: Oxford University Press; 2018.
7. Gray SM, McKay HA, Nettlefold L, et al. Physical activity is good for older adults — but is programme implementation being overlooked? A systematic review of intervention studies that reported frameworks or measures of implementation. Br J Sports Med. 2020:1–9. doi:10.1136/bjsports-2020–102465
8. Nilsen P. Making sense of implementation theories, models and frameworks. Implement Sci. 2015;10(1):53. doi:10.1186/s13012–015–0242–0
9. Tabak RG, Khoong EC, Chambers DA, Brownson RC. Bridging research and practice: Models for dissemination and implementation research. Am J Prev Med. 2012;43(3):337–350. doi:10.1016/j.amepre.2012.05.024
10. World Health Organization, ExpandNet. Beginning with the end in mind: planning pilot projects and other programmatic research for successful scaling up. 2011.
* Criteria: a study of a physical activity or exercise program for people 60+ years; the researchers measured how much physical activity the older people completed with a validated measure; the study reported an indicator of implementation and/or a framework that guided the implementation of the program.

